Alcohol Dependence

Acamprol Tablet (Acamprosate)
Packaging : 6 tablets in 1 strip
Manufactured By : Sun Pharma ...
Our Best Price : $0.69 /Piece
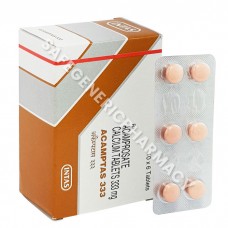
Acamptas Tablet (Acamprosate)
Packaging : 6 tablets in 1 strip
Manufactured By : Intas Phar ...
Our Best Price : $0.70 /Piece
Disulfiram 500mg Tablet (Nokrono)
Packaging : 4 tablets in 1 strip
Manufactured By : Kachhela M ...
Our Best Price : $0.40 /Piece
Esperal 250mg Tablet (Disulfiram)
Packaging : 10 tablets in 1 strip
Manufactured By : Torrent Ph ...
Our Best Price : $0.42 /Piece
LDN 1.5mg Capsule (Naltrexone)
Packaging : 10 Capsules in Strip
Manufactured By : Centurion ...
Our Best Price : $0.44 /Piece
LDN 3mg Capsule (Naltrexone)
Packaging : 10 Capsules in Strip
Manufactured By : Centurion ...
Our Best Price : $0.66 /Piece
LDN 4.5mg Capsule (Naltrexone)
Packaging : 10 Capsules in Strip
Manufactured By : Centurion ...
Our Best Price : $0.79 /Piece
Lodonak 1.5mg Capsule (Naltrexone)
Packaging : 10 Capsules in Strip
Manufactured By : Kachhela M ...
Our Best Price : $0.44 /Piece
Lodonak 3mg Capsule (Naltrexone)
Packaging : 10 Capsules in Strip
Manufactured By : Kachhela M ...
Our Best Price : $0.66 /Piece
Description
Alcohol Dependence